Use of healthcare IoT devices for sensing patient vital signs enables fast and cost-effective remote monitoring of patient safety and data quality – however the challenges start after collecting the data.
Healthcare IoT for sensing patient state is not a panacea.
Monitoring of data you collect in your clinical trial using healthcare IoT requires up-front planning and preparation but also the ability to respond to bad news and unexpected events.
In this article, Jenya Konikov-Rozenman surveys the 3 elements you need to implement to ensure success in use of healthcare IoT devices in your clinical trials.
Planning for success for your study monitoring activity with healthcare IoT
There are 3 pieces to successful monitoring; by adopting a holistic approach with all 3 pieces you will save time and improve your chances for success.
Understand the monitoring tools at your disposal
In the last few decades the number and complexity of clinical trials have increased dramatically especially as medical IoT become more prevalent – for example use of a mobile glucometer to collect blood sugar and feed it directly to the EDC system.
Sponsors of clinical investigations such as human drugs, biological products, medical devices and combinations must ensure not only the quality of clinical data submitted to FDA and EMA but also devote attention of the safety, welfare and protection of the rights of subjects in the trials.
Regulatory agencies such as FDA require sponsors to monitor the conduct and progress of their clinical trials and use of healthcare IoT does not reduce the importance of this requirement.
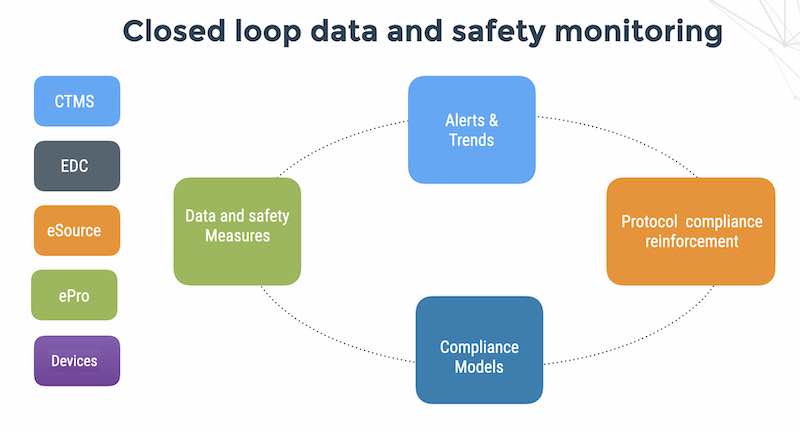
Monitoring plans should detect important risks to human safety, data quality and address the challenges of oversight taking advantage of modern cloud-based technologies.
The 3 types of monitoring
Monitoring is a quality control tool for determining whether study activities are being carried out as planned, so that deficiencies can be identified and corrected. There are 3 types of monitoring – all 3 should be part of your holistic plan for study success.
1. Onsite monitoring is like carpet bombing your sites
On-site monitoring is when a sponsor or representative of him comes to the sites and identifies data entry; compares between the data in source documents and the data entered to the CRFs; provide assurance that study documentation exists; assess compliance with the protocol and investigational product accountability; assess the familiarity of site’s staff with the protocol and the investigational product. On-site monitoring can be helpful in early study stages and in case of a complex protocol with novel procedures with which the site stuff is not familiar. On-site monitoring and 100% SDV is an ineffective, expensive and inefficient process for multi-center trials with more than 2 or 3 centers or trials with more than 200 subjects. In other words – onsite monitoring is the equivalent of carpet bombing.
2. Remote monitoring technology with healthcare IoT
Remote monitoring with healthcare IoT exceeds the capabilities of on-site monitoring, since it enables real-time data collection. FDA guidance for Risk-based monitoring stresses the use of modern technologies for remote monitoring, automated detection and response to deviations.
It has been reported by Bakobaki et al. that remote monitoring activities could have identified more than 90% of findings identified during on-site monitoring visits.
It is recommended to design a monitoring plan that is tailored to the specific human safety and data integrity risks of the trial. Remote monitoring is the equivalent of a sigint (signal intelligence) that enables identifying the threat and later dispatching a drone or small military unit to neutralize the threat.
3. Human intelligence
There is a story that made the rounds after 9/11 that the CIA had 1 person stationed in Saudi Arabia and that he had a sign over his desk – “Better to do nothing than to do something and get caught”. At the time – the Americans were relying almost entirely on signal intelligence and their satellites. And as history showed us – was not a good approach for mitigating the threat of Al Qaeda.
Connections with people on the ground in your sites is a supremely important factor in identifying problems and remedying them quickly. A weekly or monthly phone call to the site CRC and PI will help support them on their ongoing clinical trial operations and also enable you to hear first-hand about problems with the product, your EDC system and your procedures. This can be supplemented with a direct hot line to the sponsor. There are some great cloud technologies to do this sort of thing for cheap – check out fone.do!
The role of risk assessment
When you build your monitoring plan – do a risk assessment. Consider your most important assets in the study (subject safety, primary endpoint, adverse events, recruiting rates), consider threats to those assets (for example – under or over dosing that can threaten both safety and compliance to your study protocol). Try and estimate the probability of these threats and consider cost-effective controls (for example – remote monitoring of the patient dosing over time and a visual dashboard that shows the sponsor’s monitoring team what sites are violating protocol with wrong dosing and how often it’s happening).
But there is a caveat to this.
Risk assessment is not a one-off activity
Never forget – medical device clinical trials are a scientific experiment. Surprises, problems can always happen and you need to keep your finger on the pulse of the study in order to recover quickly and proceed with the trial. Risk assessment is not a static activity – and reevaluation of risks will be inputs into changes to your procedures, protocol and your EDC system.
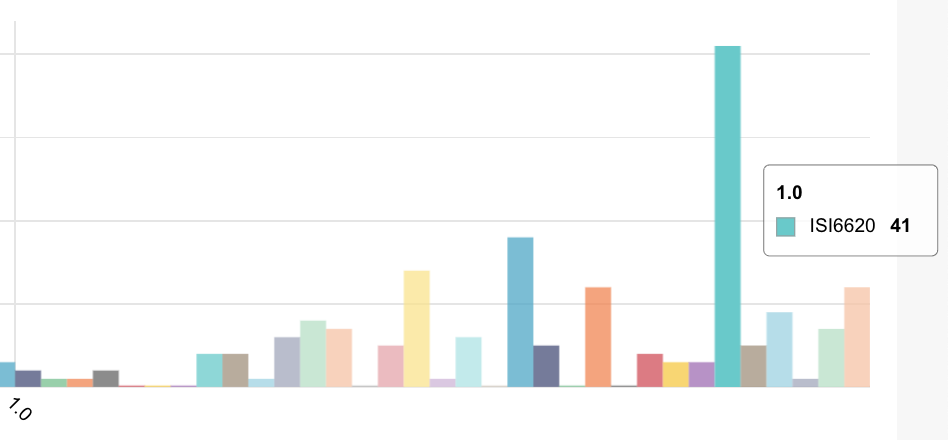
You may not be able to even do a risk assessment at the beginning of the study – and may very likely have to collect enough data in order to even know what areas are problematic and where things are going wrong. This illustrates how collecting monitoring data needs to be done before your risk assessment.
In summary.
Monitoring is a continuous and essential piece of your study success especially when using healthcare IoT for sensing the patient state.
Monitoring is part of the ICH/GCP regulatory requirements for data quality, patient safety and patient compliance to the study protocol. A successful monitoring operation will combine effectively (and for your business situation) all 3 types of monitoring – technology-enabled remote monitoring, escalation to onsite resolution of problems, and ongoing human interaction with your sites.
Jenya Konikov-Rozenman has a masters degree in biotechnology from the Hebrew University and is a doctoral candidate at Tel Aviv in medical science working on basic science in Duchenne.
She is GCP and CRA certified and leads FlaskData product development with super-human devotion to delivery. Jenya dances and skis in her spare.