This is a post David wrote a while back and it still seems relevant. If you would have asked me 2 years ago – I would have told you that in 2018, no one would be doing paper medical device clinical trials the same way that no one does paper accounting. I would have thought that logic would prevail considering the advantage of using automation and technology instead of using your Chief science officer to manually enter data into Excel.
Medical science is the foundation for innovative medical devices. Taking medical science and developing a medical device product requires translating basic science into technology. This is self-evident.
So why do so many innovative medical device vendors conduct their clinical trials using paper? Damn if I know. Using paper for medical device clinical trials is somewhere between penny-wise and pound foolish and plain dumb.
Every year, 20,000 clinical trials are performed. An electronic data capture (EDC) system is quickly becoming adopted as the modern standard for monitoring in clinical trials. EDC solves the problems that are inherent to traditional, paper-based methods of data capture. During medical device clinical studies, the accessibility to real-time data capture and storage during conduction is key to performing a study that is cost efficient, and effective in generating results.
Paper-based = slow and costly
EDC = quick and efficient
Do not forget these simple equations, as they should become your mantra.
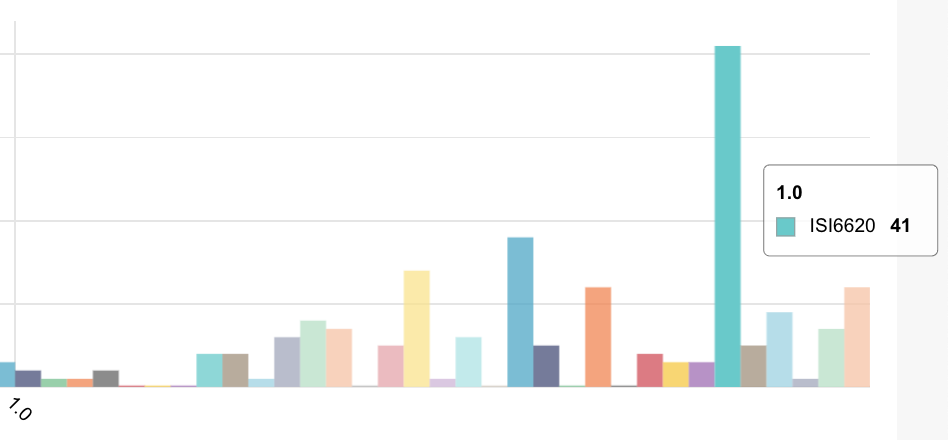
As seen below, the number of medical device clinical trials conducted is like the global population; it only keeps increasing. The pressure is on for product developers to conduct studies in the most expedient fashion possible, and collecting data that is not only pertinent and useful, but is clean and devoid of doubt concerning its accuracy.

Thanks to technological advances (read: EDC), on-site monitoring and clumsy, paper-based data storage are going the way of the dodo bird. The use of EDC as a basis for automating patient compliance during medical device clinical trials is quickly developing as more an more medical devices become connected via mobile and home wireless networks.
Paper-based data capture systems are irrelevant for connected medical clinical trials.
90% of drug development costs are invested in clinical trial conduction. EDC systems facilitate automation of patient compliance during the duration of the medical device trial. And while not every medical device trial uses connectivity and automated patient compliance monitoring, there is an increasing understanding that the direction is digital and not paper.
The majority of the public values clinical trials for the healthcare industry, as seen below. Implementing an EDC system for medical device clinical trial monitoring has proven to reduce study costs by 59%. So, ask yourself, what are you waiting for?

As seen above, the value of clinical trials is understood by the public, and as clinical trials continue to grow in scope of variables and number of participants, they require a more efficient means of data capture in order to cut the costs involved in monitoring. EDC systems provide exactly that. Here we will touch upon why an EDC system is becoming an essential for clean and efficient risk-based monitoring in clinical trials.
Medical device monitoring data is available in real-time
Using an EDC system affords the opportunity for study monitors to receive data entered by clinicians as soon as it is collected. By using hand held devices, such as a tablet, that are logged into an EDC system, makes risk-based monitoring a breeze. No longer does one need to record data on a clipboard, and then duplicate the same data into an on-site hard drive. This means that monitors are getting their hands on information the second it is captured.
Simply put, the faster that you get data into the hands of your monitors, the greater the efficiency of the study.
Increased study efficiency through cloud notifications
Recently, for the past 20 years or so, medical device clinical trials have been substantially increasing in scale and complexity as they continue to become more valued and salient as a means of biomedical development. Often, they involve a sizable number of people responsible for entering data, and study monitors assigned the task of monitoring specific variables and patient compliance to the protocol.
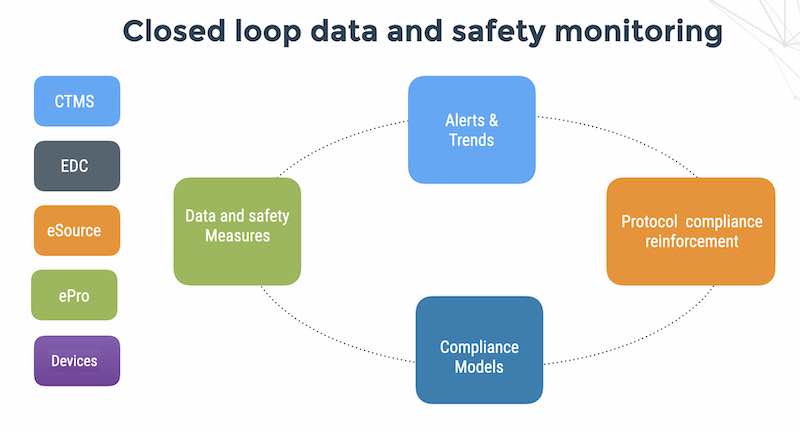
An EDC system automates the appropriate delivery of fresh and high-quality data from investigational sites, patients and connected medical devices. Whoever needs to receive whatever data variables from a clinician are notified in their personal account via the cloud. Not only does cloud-based EDC keep monitors informed in real time, but the organization and delivery properties ensure that the right monitors are receiving the right data, increasing efficiency in increasingly complex studies.
When data is entered after capture, an EDC system can automate from the entry user the delivery of data to the assigned monitor. Email alerts can also be integrated into the EDC system, so that whenever data is entered for review by a monitor, they are informed even if they are not logged into the EDC system.
Reduced monitor travel costs with remote compliance monitoring
Not only does using EDC keep monitors informed of new captured data as soon as it happens, reducing subject risks, but monitors can perform their tasks from abroad, saving travel time and expenses. The features of using a cloud-based EDC system are nearly endless, but the decentralizing of on-site data monitoring is one of its greatest boons.
Monitors that work from home going to be willing to receive lower salaries, and people are generally happier when they can work from home. Your study will save time and money by an increased retention rate in monitor personnel, that are willing to work with a clinical trial sponsor, study after study.
Further, and this is a benefit from remote monitoring of your medical device clinical trial that most would not think of, consider reduced human traffic at your study site. The less people you have at your study site the better, as there is simply less for on-site study managers to focus on. This is a minor benefit of an EDC system, compared to the speed of data delivery with EDC, but a benefit nonetheless.
Also consider that remote monitoring can allow the outsourcing of monitors. If your study site is located in California, but there’s a team of specialists in India, willing to perform exceptional quality of monitoring for lower salaries, of course you are not going to fly them over to work for you; cost prohibitive. If you are using the standard on-site monitoring method that comes with paper-based systems, your resources are limited to only those that can geographically travel to your study site.
Cleaner, consistent data submission to monitors
EDC systems can use a study-specific standardized data collection form, reducing errors in collection and delivery to monitors. Consistency is key to running a smooth, hassle-free medical device clinical trial. By using standardized electronic data collection forms, your study will erase the possibility for inconsistent data submission from data managers to monitors.
Paper-based data capture systems may seem familiar and comfortable to clinicians, and making the transition to an EDC system may seem like a plunge into unknown territory, but the data is plainly cleaner when conducting a study with EDC. The deficit of errors and omissions that are caused by implementing EDC are a tremendous ROI for your study. Consider the following:
For example, in a paper-based system, data is recorded by hand, and even something as seemingly trivial as handwriting comes into play and can muddle data. Not every clinician will have the best penmanship, so this opportunity to corrupt data is entirely circumvented by using an EDC system.
A more frequent, and damaging, corruption of data that occurs when using the standard paper-based system are data errors and omissions when recording data. People make mistakes, for whatever reason. It is natural, and bound to happen. Say, for instance, that you have a subject XY-1001-9, for which the clinician is collecting data; it is very easy to write YX-1001-9, XY-101-9 or XY-1010-9 if a clinician is distracted, or maybe just operating on little sleep from the previous night.
By working with an EDC system with standardized data collection forms, the above scenarios are entirely avoided. That being said, standardized forms are not going to write themselves. During the planning stage of your study, devote time to organizing and developing the standardized form model you are going to use for each subject in your study to reduce errors and omissions. In the long run, your ROI will go through the roof.
However, even in an EDC system, mistakes can be made. No system is entirely error-proof, especially when being implemented for the very first time. When a mistake inevitably does happen, it is far less of a headache to solve and prevent from recurring using an EDC system. For starters, FDA compliance adherence measures should already be in place at the hands of the EDC software vendor. As compliance standards are modified by the FDA, they can be updated in the EDC system without a hitch. When data entry errors occur, they can be addressed by programming the software to recognize proper form entries.
Another feature of EDC systems for reducing errors and omissions is data entry recognition standards. Remember the subject number examples? If you write something down on paper, there is no real way to tell if you got it right the first time, than somebody else telling you who has noticed that you have made a mistake, and then correcting it themselves. Every field of the EDC user interface can be programmed to recognize whether the data entered was in the proper format, and whether any fields were skipped or not submitted.
An EDC system also reaps tangible data capture benefits for studies using subject-submitted data. Many subjects are not experts in clinical trial data management and entry, and unless you are conducting a study into only a single variable, patient submitted data, which saves time and costs, is an impractical approach to collecting study data. However, whilst being cloud-based, EDC allows any subject with a smartphone, tablet or computer the ability to submit data, at the very moment it is noticed and measured, mitigating subject risks and saving on study personnel expenses.
For user submitted data, the standardized data collection form with checks in place for data submission ensures that the subject will not make a mistake when submitting data. You will be able to get by and hire less clinicians for future studies, a further cost saver of EDC.
Facilitating future medical device studies
After you take the plunge (and please do, ASAP) into EDC and forego paper-based data capture, the benefits will be noticed immediately for your next clinical trial. Not only will every facet of your data capture and monitoring be smooth sailing, but think of the future studies you will be sponsoring, and how they will benefit.
Not only does EDC facilitate the aforementioned features, but after you and your study personnel (and subjects if applicable) are trained and familiarized with the use of the EDC system you have chosen, future studies will be up and running faster than you can say “outdated, paper-based data capture.”
EDC systems significantly cut the time spent during the planning and preparation phases of a medical device clinical trial. Consider how while you are planning the variables and factors to be measured, you can instantly enter them into the software, saving time and money that would otherwise be spent on designing paper forms and making copies. EDC systems are flexible, and if study personnel is trained properly by the software vendor from the get go, require little maintenance for their design.
What are you waiting for?
Hopefully you now have a better understanding of how vital an EDC system is for an efficient medical device clinical trial, and how many headaches it alleviates for monitoring clinical trials. When you are looking for a vendor, ask how they can eliminate rework and detect problematic trends in real-time. Ask them if they require expensive third-party analytics and if they limit the number of users that can use risk-based monitoring tools and make sure they have a great training program. Enjoy your streamlined future studies.