In this post, Danny Lieberman, founder of flaskdata.io , discusses when patient compliance is crucial for your medical device clinical trial and when patient compliance is a negligible factor to success of the study.
From adverse events to patient compliance
My original goal for Flaskdata.io was to use machine learning to predict onset of adverse events during interventional medical device clinical trials.
For that goal, we needed data, so we started by providing cloud EDC services for medical device clinical trials with high-touch personal service and attention to the quality of the data model. Very quickly – it become apparent that we did not have enough data (and after 20 studies, hundreds of sites and thousands of patients), we still do not have enough data to predict adverse events.
However, after performing 6 digital clinical trials in 2 chronic disease indications (acute migraine and chronic constipation) we had an epiphany – “PATIENT COMPLIANCE IS KING”.
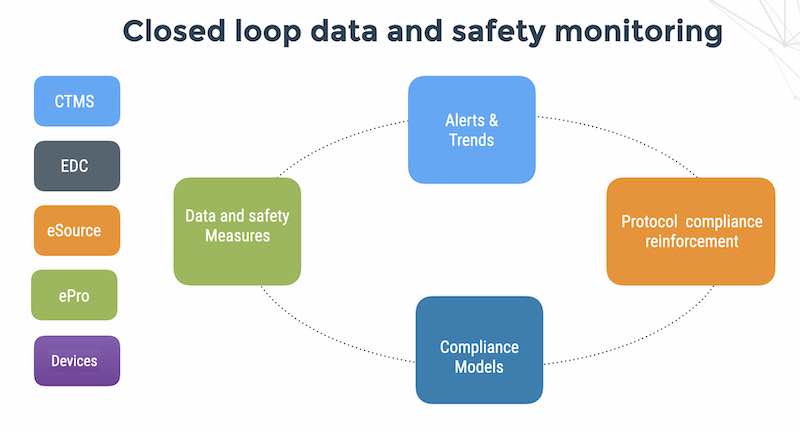
Customers using the Flaskdata.io platform for digital clinical trials, collected data via the EDC from investigators, collected data from patients (via our ePRO app) and collected data from connected medical devices (via the Flaskdata.io medical device API). The evidence was overwhelming :
Patient compliance to the protocol is an acute issue and critical success factor to the success of a connected medical device clinical trial.
Or is it.
Who owns patient compliance? The sponsor, the CRO, the site or the subject?
This discovery of the importance of patient compliance made a profound impression on us because it came from customers and empirical data they collected in our EDC systems. This impression would not change, although we began to hear dissenting opinion on the importance of, and responsibility for patient compliance in clinical trials.
Public discussion on trends in the clinical trials industry is heavily influenced by big pharmaceutical companies, big CROs like PPD and IQVia and a $70BN/year clinical operations services industry that deal largely with oncology and biotechnology. When we spoke to biotech prospects about the ability of our digital clinical trials platform to accelerate time to regulatory submission and assure high levels of patient compliance – people smiled and said “Well automated compliance monitoring is an innovative approach, but in fact, patient compliance is not important to us”.
We then spoke with the Israel country manager of one of top 3 global CROs – and they said “Interesting question. We collect many clinical trials operations metrics, but patient compliance to the clinical protocol is not a metric we collect”. I asked – “In that case, who is in charge of patient compliance? and the answer was – the sites”. In this scheme of things, if patient compliance is not a CRO metric, then the sponsor has a blind-spot to what is possibly, the single most important factor to the success of his connected medical device clinical trial. Or not.
After that, we spoke with the country manager of one of the top 3 pharmaceutical companies and Israel and he told us again “Patient compliance is a non-issue for us. Patients come to the hospital and get treatment and there is no problem”. I asked him “What about psychiatry trials?” He replied – “well yes, everyone knows that psychiatry trials have acute issues of patient compliance”
Hmm.
We then went back and did the most logical thing – searching in Google for “the critical success factors of clinical trials” and there are 290 million results and a ton of empirical evidence and academic and industry research on the importance of patient adherence in clinical trials.
And this vast body of empirical data is dealing primarily with drug trials, not medical device trials. The VP Clinical of a gene therapy prospect (who had previously worked at a medical device company) told us that in gene therapy patient compliance is negligible while in medical device trials, patient compliance is acute.
Hmm again. So what does Google say?
The high failure rate of clinical trials has significant impact on providing potential curative treatments to patients in need….
One key factor that has been identified in the high failure rate of clinical trials is the adherence of patients participating in clinical trials to the dosing, treatment, and study procedures that are very carefully put in place in clinically rigorous protocols. Due to the rigor that is required in order to demonstrate an “effect” relative to a standard of care treatment, even a small deviation in medication adherence can result in a trial failing to meet its pre-specified clinical endpoint.
Additionally, the current nature of clinical studies include strict timelines and competition among sites to enroll eligible subjects which can many times result in the inclusion of subjects that are simply not “medication-compliant”. The issue of medication adherence is therefore one key factor sponsors should carefully look at monitoring closely when designing and planning the medical and operational oversight of their trials.
Unfortunately, the issue of medication adherence many times goes unmanaged and falls solely on site staff to oversee. As clinical sites are many times running multiple concurrent trials and are themselves pressed to remain productive, the one-on-one daily management of medication adherence of study subjects can many times be neglected. It is therefore in the best interest of the patients in need that sponsors look towards solutions that can help to support their clinical sites in providing additional resources to maintain close and frequent interactions with subjects enrolled in key studies. It simply is no longer sufficient to rely solely on very busy clinical practices to ensure successful adherence of patients in enrolled in trials.
See Compliance – a key factor to a successful clinical trial.
I’m confused. Is compliance the best interest of the patient or the best interest of the PI, or the sponsor or all of the above? We know that the PI must monitor participants’ compliance with study requirements. Failure to monitor patients adequately can sabotage the entire study and damage the site’s reputation.
CROS not collecting patient compliance metrics. Busy sites. Lack of tools. PIs who are generally not hands-on with the patients. Sounds like a classic finger-pointing situation.
We hear of the importance of site selection, but if patient compliance is not a CRO metric, then how do we measure site performance properly?
The 4 quadrants of patient compliance
In fact, the question of HOW to measure the importance of compliance is intimately related to 4 factors – and interestingly enough is totally unrelated to the site or the PI. The 4 factors of patient compliance are:
1. How do you collect data?
2. What is the indication?
3. What does the product do?
4. How involved is the patient in the treatment?
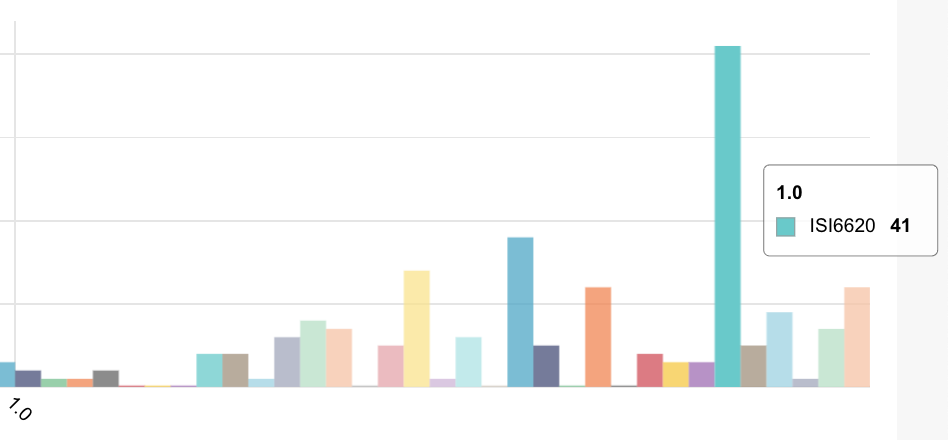
In order to understand why there is dissenting opinion on the topic of the importance of patient compliance – we can map life-science products into 4 quadrants: (Patient-centric, Digital, Investigator-centric, Implanted). The top right quadrant in green is a digital clinical trial for chronic disease, the top left is a traditional EDC operation with varying degrees of patient involvement, the bottom left is little patient involvement and EDC data collection from paper source and the bottom right is no patient involvement but with data collection from implanted devices (an interesting and extremely important use case in its own right).

The above picture tells the whole story.
Patient compliance in clinical trials is crucial in digital clinical trials and patient-centric trials using traditional EDC and patient reported outcomes.
In the end it is about the patient – not the PI, not the site operations team and their training, policies and procedures and not about the CRO.
But hey – this is something any sponsor worth their salt already knows.