A widely neglected factor in cost-effective risk-based clinical trial monitoring is availability and accessibility of data.
RBM methods used by a central clinical trial monitoring operation that receives stale data (any data from patients that is more than a day old is stale) are ineffective. Every day that goes by without having updated data from patients, devices and investigators reduces the relevance and efficacy of remote monitoring.
Real-time data is a sine-que-non for RBM.
Sponsors and Contract research organizations (CROs) should therefore approach real-time data and risk-based monitoring (RBM) as 2 closely related priorities for executing clinical trials. Use of modern data technologies for real-time data collection and remote risk-based monitoring will reduce non-value added rework, people and paper in clinical trials and help speed up time to statistical report.
The goal of any clinical trial is to test the efficacy and safety of innovative pharmaceutical products and medical devices that improve quality of life, cure disease and protect patients.
CROs are charged with the task of conducting clinical trials that are valuable to the healthcare industry and produce real results. RBM helps assure that data collected is reliable, and can be applied to help develop innovative drugs and medical devices by reducing patient safety and data quality risk in studies.
In this post, we are going to go over how real-time data and remote risk-based monitoring will help your current study and also provide value for future drug and medical device development.
Risk-based monitoring entails the mitigation of risks during a clinical trial that a CRO is conducting through the process of identifying, assessing, and then monitoring the risks associated with patient safety throughout the course of the study.
In August 2013 the FDA issued draft guidance for “A Risk-based approach to monitoring”. The overarching goal of this guidance is to enhance human subject protection and the quality of clinical trial data by focusing sponsor oversight on the most important aspects of study conduct and reporting”
The draft guidance includes three steps in a risk-based approach to monitoring:
Step 1 – Identifying critical data and processes. To accurately monitor the quality of a study and the safety of its patients, sponsors must know which elements are vital for each particular study, including informed consent to eligibility screening and tracking of adverse events.
Step 2 – Performing an assessment of risk. Risk assessments requires determining specific causes of risk and the effect of study errors pertaining to risk.
Step 3 – Developing a comprehensive monitoring plan. According to the FDA’s guidance regulations, RBM plans should “describe the monitoring methods, responsibilities, and requirements of the trial.” Planning is responsible for communicating risks and monitoring procedures to each party involved in trial RBM.
Real-time data using eSource, ePRO and connected medical devices
FDA guidance is clear on what constitutes eSource:
Data can be entered into the eCRF either manually or electronically (from ePRO and connected medical devices) See FDA Guidance for eSource
Direct Entry of Data Into the eCRF
Many data elements (e.g., blood pressure, weight, temperature, pill count, resolution of a symptom or sign) in a clinical investigation can be obtained at a study visit and can be entered directly into the eCRF by an authorized data originator. This direct entry of data can eliminate errors by not using a paper transcription step before entry into the eCRF. For these data elements, the eCRF is the source. If a paper transcription step is used, then the paper documentation should be retained and made available for FDA inspection (see section III.A.2.c).
When eSource documents, ePRO and connected medical device data are accessible in real-time in the cloud EDC, remote monitoring and automation of patient compliance becomes possible.
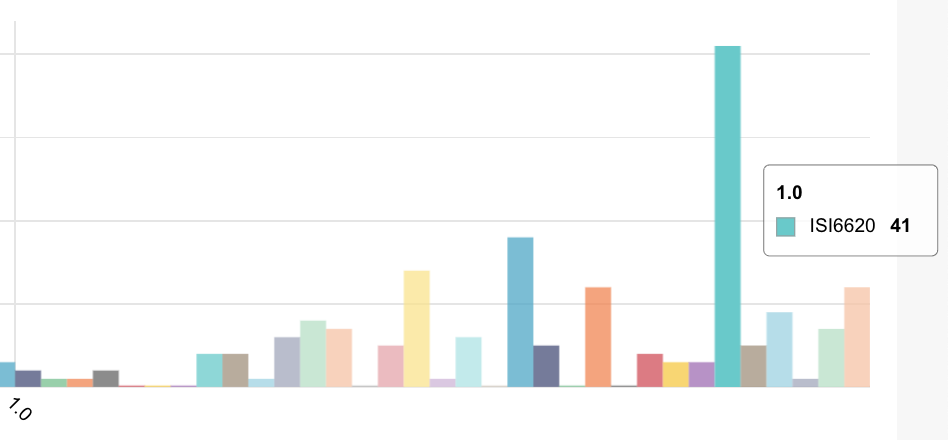
Remote risk-based computer-science monitoring algorithms are designed for scanning the data for specific and calculate specific metrics that trigger alerts to the clinical data management team – for example excessive query rates or the cycle time from patient visit complete to eCRF data entered both of which are indicative of data quality issues at sites
Remote risk-based monitoring metrics fall into 3 categories:
Note that all 3 are related directly or indirectly to patient compliance
1. Patient compliance to the protocol (whether at home or in a clinic/hospital)
2. Patient safety risk (for example trends of vital signs) related to patient compliance
3. Data quality risk (for example low levels of reporting compliance to the ePRO)
When study monitors visit sites once every 2-4 months, it is impossible to catch slow-moving, high risk events. Human brains are not good at identifying and classifying small numbers of slow-moving events, although they can easily identify a face moving quickly across a basketball court.
Computer algorithms are outstanding at identifying anomalies in time-based clinical data found in clinical trials – and this is where RBM will have its biggest payback for you in your study.
What comes next?
What comes next is to make an accurate assessment of the data model. A single number, or a graph displaying data points, data in any form, has no meaning until the data is coherent and understood by a clinician with how the data is understood, and interpreted with how it can produce increased or mitigated risk to the patient, and the study as a whole.
RBM and real-time data are key to automating patient compliance to the protocol
Take this for example: if the automated compliance monitoring system reports poor reporting compliance by patients – is this a failing of training, the site coordinators or a result of issues with the treatment – where patients have side effects. In the last case – the automated compliance monitoring metrics will include adverse events reported at the same time as the PRO (patient reported outcomes).
The RBM system will alert you in real-time to signals over or under threshold in order to enable the clinops team to dive in deeper, and alert study monitors to observe the monitoring signals and ascertain if there are issues with site compliance, patient compliance or treatment performance.
eSource (and paper reduction in general in your study) together with compliance automation are essential components in your RBM process.
eSource (entering data directly into the EDC) guarantees timely data collection, reduction of non-value work on SDV and ability to automate calculation of compliance metrics that indicate levels of protocol compliance risk –
without having to perform time-consuming and error-prone data extracts and analysis.
The next crucial course of action during the study is to use the findings to take a direct course of action. With a clear understanding of a site’s specific risk level, site monitors should be tasked to visit the site(s) and take appropriate measures to mitigate patient protocol compliance issues.
With a coherent and thorough understanding of study risks, CROs and sponsors can take the necessary steps to not only reduce current study patient compliance risks, but reduce future patient compliance risks, helping your studies run more efficiently and save future costs.
Our experience with at over 350 global sites shows that the combination of real-time data collection with eSource from clinical research coordinations, ePRO from patients and automated data feeds from connected medical devices for biometrics is a must for automated compliance monitoring and implementing a cost-effective RBM system for your study whether executed by a CRO or directly by the sponsor
Look out for these outliers
1. Fabricated, false data
2. Data omissions
3. Patient compliance deviations from protocol
4. High rates of queries (a proxy for poorly training site coordinators or poorly-designed EDC)
5. Inconsistent procedure between sites (for example CRCs who SDV the eSource and ePRO data)
6. Unusual changes in vital signs. Take for example if there was data that showed an alarmingly high rate of a rise in blood pressure for study subjects. Monitors should not only be looking into the increase in blood pressure, but also examining whether the data being submitted is accurate. Monitors should think about whether the submitted data is wrong, or if the data is sound and the root cause of vital sign deviations is due to treatment.
Real-time data and RBM as drivers for continuous improvement
1. Real-time data from eSource, ePRO and connected medical devices is the basis for any remote monitoring system.
2. Real-time and RBM is a culture for study operations.
3. The goal is patient compliance and continuous improvement in clinical operations as measured by faster times to submission and reduced CRO costs.