A comparison between pharma trials and medical device clinical trials

The differences between medical device trials and drug efficacy studies are similar to the differences between starting a law firm and starting a business training runners – while both are businesses in a basic sense, they each have specific criteria to adhere to regarding government regulation of standards and practices, and varying endpoints to determine whether the customer/client is satisfied and a task is finally complete.
There is also a vast difference in numbers and uses. More than 500,000 different types of medical devices are produced globally – compared to 20,000 medicinal products – each in service of vastly diverse indications.
For the law firm – regulatory compliance impinges on the lawyer and for running – compliance hinges almost totally on the runner.
But the analogy is not arbitrary. Pharma trials are like law firms – where protocol compliance is primarily the responsibility of the principal investigator. Trainers are like medical device trials – where protocol compliance is primarily the personal responsibility of the runner (the patient).
Before we examine and reveal whether or not clinical monitoring of medical device trials is easier than clinical trial monitoring for pharmaceutical trials, it is better to understand that first of all they are significantly different from one another.
Simpler, or just different?
During pharmaceutical testing, extensive clinical trials are necessary to evaluate the efficacy and safety of each and every drug, every single time pharma develops a drug in hopes of bringing it to market. With regards to medical devices, some do not even require a trial whatsoever. For example, a simple bandage is indeed considered a medical device, and subject to regulatory body regulation. Yet, a bandage for protecting a healing, minor laceration will not require a clinical trial during design and development.
When we refer to a “medical device”, it is a blanket term and can refer to everything from gauze or scalpel to a prosthetic limb or stent. For devices that pose a risk to patient safety, a trial must be conducted. That being said, while every drug needs to be tested through Phase I to Phase III, and monitored after it is brought to market during Phase IV, medical devices that pose minor risk to patient safety do not require the degree of testing that higher risk devices do.
While many medical devices are exempt from clinical trials pre-marketing, interventional medical devices for chronic diseases like migraine and chronic constipation require a series of clinical trials even for predicate devices. Since chronic disease involve home use medical devices – the issue of patient compliance becomes acute and real-time clinical becomes a critical success factor for the medical device clinical trial.
Given unique indications and interventions, for high-risk medical devices, such as powered units like pacemakers or radiation generators like x-rays, the clinical trials required before bringing them to market can rival pharmaceutical testing in scope and complexity. Both industries require regulatory compliance, for example with 21 CFR Part 11 for electronic record documentation and storage.
Again, it is like comparing a running trainer to a lawyer – the trainer needs to ensure that she keeps her runners on track with a safe but continuously-improving running schedule (volume and speed), and the lawyer needs to sustain a practice that meets regulatory and ethical standards. Even though each vocation presents their unique challenges, both the trainer and the lawyer need to file their taxes at the end of the year or answer to the IRS.
That being said, when all is accounted for, the trainer probably has a more challenging compliance situation than the lawyer. Let us examine this question by comparing medical device clinical trials to drug trials.
Randomization vs fixed group
One key difference during the clinical trial of a drug or medical device may be the randomization of study subjects. Pharma demands that patients be randomized when monitoring and evaluating a drug’s efficacy and side-effects, and drugs are wildly less predictable than a device.
Placebo monitoring
When developing and testing a device, regardless of whether it is an MRI or a syringe, there is no placebo to test it against – the device is either performing as expected or needs adjustments/redesign. Drugs are metabolized by the body, whereas devices simply demonstrate their functionality or not.
In this case, medical device trials are measurably simpler than their pharmaceutical counterparts, requiring less study subjects and less long-term monitoring before making it to market.
Number of study sites and subjects
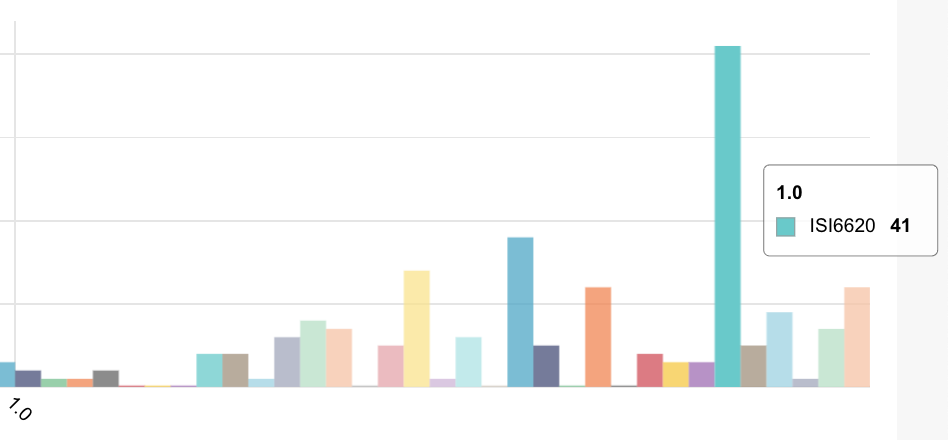
Pharma clinical studies, especially Phase II and beyond, involve a vastly greater number of study subjects (Phase III is typically in the thousands) across any number of study sites, often in multiple countries. Medical device clinical trials testing for efficacy may involve smaller numbers of sites and subjects – on the order of 10-20 sites and less than 1000 subjects. However, the somewhat lower number of subjects is more than offset by generally large numbers of variables that are collected per subject – typically as much as a 1000 variables not including repeat visits.
Blinding and clinical monitoring
Drug trials, in an effort to mitigate bias toward efficacy, are conducted using blind controls – where the patient knows not whether they are being administered an active drug or placebo, or double blind – where neither clinician nor subject are aware of placebo or drug during testing.
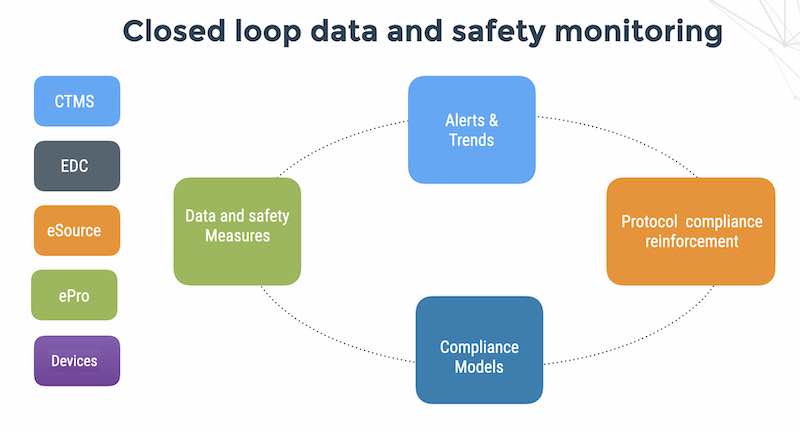
Medical device studies’ requirements for blinding and clinical monitoring in safety and efficacy studies can be quite complex with requirements for CRF and user role level blinding, in order to prevent investigators from being biased during recruitment and in order to prevent blinded evaluators such as histologists from being influenced by site findings. In this respect, medical device trials may actually have a higher level of complexity for clinical trial monitoring due to blinding requirements. When patients are blinded, ensuring patient compliance becomes a difficult technical challenge for EDC systems and generally requires a separate CTMS and ePRO system which then cascades into HIPAA and GDPR privacy requirements.
CRO staff training
With pharmaceutical clinical trials, sponsors need to ensure that staff are trained in the data capture system planned for the study, whether it is paper-based or EDC. Either way, except for brand new clinicians, monitors, managers, etc. it is far more likely than not that the CRO staff have experience with paper systems.
If switching to EDC from paper, the bulk of the data capture and monitoring logic stays the same, and minimal onboarding (2-4 weeks) is required. After being initially trained, CROs have an understanding of the system, and the knowledge can be applied to future studies without a hitch.
However, this is not the case for connected medical device studies, which are much more complex concerning CRO training. With drugs, pharmacologists do the legwork with regards to design – CROs simply run the trial, collect data, and monitor results. It is repetitive, study after study.
Medical devices are new technology each time they are studied, and the complexity and/or safety risks of some Class III devices can be staggering. A CRO with ample drug trial experience cannot apply their knowledge to a device study without first training clinicians, monitors, managers, and support staff with proper device operation. Especially for CROs not yet experienced with a device of similar nature, the device conduct training can be exhaustive and intensive, taking far more time and resources to amply familiarize staff with the device being tested.
So, truth or fiction?
The answer is – both. In many regards, device trials are simpler to conduct, but they present their own unique challenges for patient compliance that pharma often ignores – since the CRO is designating responsibility for patient compliance to the sites.
While both types of trials need to be equally compliant with regulatory guidelines, medical device trials pose sizable challenges due to patient compliance issues – whether compliance of patient-reported outcomes or whether compliance of patients to the treatment protocol.