Time is money
The economic model of a multi-center clinical trial is based on a commercial biotech/biomed/pharma company sponsoring and funding clinical research in order to prove efficacy and or safety of a new drug or medical device.
In fact, although the sponsor has the most at stake by far, in clinical trials, sponsors and sites both have a clear economic interest in productivity.
Looking at money – as a rough yardstick of your clinical trial budget – 1/3 will go to the investigative sites, 1/3 to the patients and 1/3 for clinical monitoring.
1/3 for clinical trial monitoring is a lot of money. How do you optimize that and make the investment cost-effective and time-effective while ensuring a high level of patient compliance to the study protocol?
Technology that makes the work-flow of data collection and clinical monitoring more effective enables the PI (principal investigator) and his/her team to be more “profitable” and comply with GCP with less effort. Complying with GCP, having more patients who adhere to the study protocol enables the sponsor to sustain statistical power for the study with less time and money spent on recruiting more subjects.
Faster, cheaper and higher-quality data collection and monitoring on demand reduces queries and site visit monitoring costs for the sponsor and enables faster data processing for interim and final statistical analysis.
In addition to cost-effectiveness – a sponsor has a supreme interest in getting the interim and final statistical analysis as soon as possible in order to understand if the trial succeeded or not. For many companies and business units – this is a make or break period.
Clinical trials account for 60% – 70% of the time invested in drug development, and 90% (yes, 90%) of the costs of developing a drug. With the advent of electronic data capture (EDC) software systems, many clinicians are gaining awareness in the time and cost saving benefits from incorporating such a system into their studies.
In this article – we will take a look at 5 dimensions of speed, data quality, costs, security and site monitoring and show how cloud EDC provides significant process improvement and cost reduction in all 5 areas.
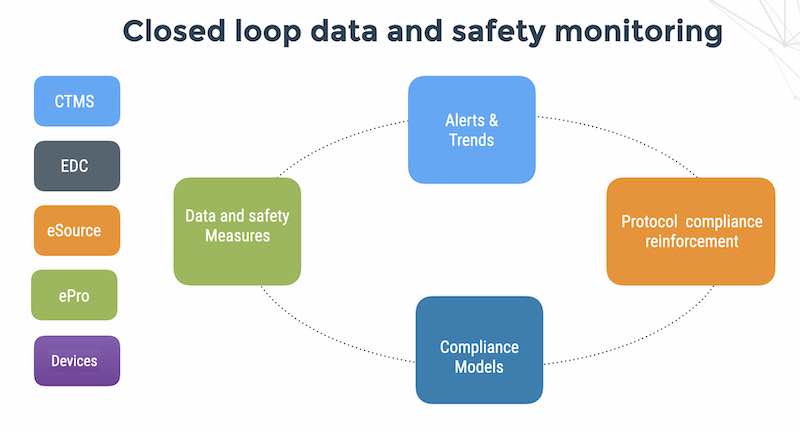
Clinical data management is multi-step process that can benefit from protocol compliance automation as we can see below:
– Patient recruitment
– First visit, patient included or excluded from the study
– Screening and follow-up visits by patient according to the study protocol
– Data collection using EDC, ePRO (for patient reported outcomes) and connected devices.
– Clinical data management “cleans” data (primarily a function in paper CRF)
– Queries, notes and discrepancies are reported by the CRC (clinical research coordinator)
– Queries, notes and discrepancies raised by study monitors during sites visits and
– SDV (source document verification)/ SDR (source document review) activities
– Drug coding, adverse event coding,
– SAE (severe adverse event reporting)
– Protocol amendments in the middle of the clinical trial that require amending the CRF
– Data analysis for interim and final reports by the study biostatisticians
– Medical writers that produce a clinical study report
– Submission of study report to FDA
With paper-based data capture, the process is not only clumsy (especially for larger, longer duration studies, with the large amounts of paper that need to be organized and transported), but also error-prone as off-line error-checking and double data entry inevitably leads to errors that reduce efficiency and increase costs and time spent on data capture.
The best biomed and biotech companies in the world all use EDC , because it saves time, lowers costs, and enhances efficiency for conducting multi-center clinical trials.
EDC systems can save overall costs by 20% – 28% over standard paper-based data capture.
Paper CRF and manual data processing is the way other industries did business in the 80s and even so – EDC is looking old hat to innovative researchers who look to even more innovative technologies like Apple HealthKit to collect patient vital signs, and treatment compliance using smartphones and mobile app and facilitate enrollment and clinical monitoring in multi-center studies.
Paper is slower, dirtier, more expensive and less secure than data in the cloud.
Here are 5 ways that cloud EDC can help you run faster, with higher data quality, better security, lower costs and better protocol compliance.
1. Faster data
Paper is slow. It can take up to 3 months for paper to reach the sponsor and the clinical data management team from sites. This is a time of low visibility of site performance, data quality and patient safety.
In the cloud the data is accessible, visible and actionable in real-time.
2. Higher data quality
In cloud EDC, data is validated as the user enters the data. When the user hits send on the secure Web form – he already knows the results of on-line edit checks for ranges of numbers, dates, and consistency with other visits ( Was a lab test at the previous follow-up visit consistent with the findings in today’s visit? Are we trying to record an event in the future?)
In the cloud the data is validated at the point of entry.
3. Better security and regulatory compliance
Consider security. A study with 20 CRF pages, 100 subjects and 5 follow-up visits generates 10,000 pieces of paper. With double data entry multiply by 2. You have to provide physical security for storing and accessing the paper. If you lose paper – the data is lost.
Consider accountability and traceability. The regulatory requirement for separation of duties means that a study monitor should not be able to enroll patients and enter CRF data. With paper everything is possible, whether on purpose or by mistake.
Paper audit trails are expensive, slow and cumbersome. An 21 CFR Part 11 compliant cloud EDC system incorporates an electronic audit trail, enabling traceability and understanding of how and why data values got to where they are.Errors will happen, but with EDC they are identified and corrected with much greater efficiency than a paper-based clinical data management system.
4. Cheaper than paper
The numbers speak for themselves. A paper-CRF based study costs in the range of USD 1,000-1,500 per subject. 100 subjects is $150,000. In cloud EDC, the monthly subscription is in the range of USD 1,500 – 2,500/month. Let’s take the higher number for a 24 month study – the cost will be $72,000 – less than half the cost of paper.
Data cleaning, query resolution and data analysis for the study may take up to 6 months. With cloud EDC and cloud monitoring as a service this shrinks to 6 weeks, saving 20 weeks of cash burn-rate – a medtech startup with 10 employees will burn $100,000/month – this is a non-tangible savings of $2M – which makes cloud EDC and monitoring a slam dunk for a small medtech sponsor.
5. Better quality, cheaper site and faster site monitoring
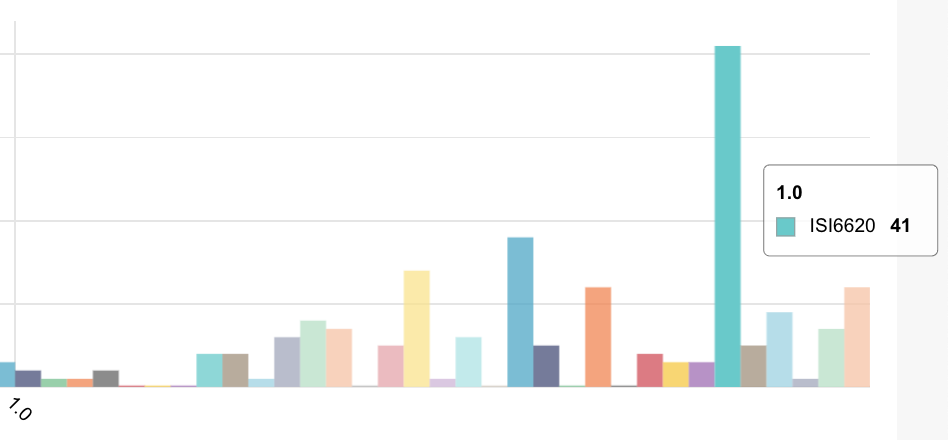
In much the same way that EDC systems have on-line edit checks of data, , the data management process can leverage remote clinical monitoring services that employs compliance monitoring algorithms that run in the cloud.
Remote monitoring in the cloud of all sites all the time, enhances the ability of the clinical data management team to detect protocol compliance issues and respond faster without having to go onsite and perform SDV.
In global multi-center trials, on-site visits are typically performed once every 4 weeks.
Global monitoring on demand is like a having a study monitor on site all the time and enables the study monitors to perform targeted SDR (source document review) when quality and compliance issues are detected at particular sites, obviating the need to physically visit all sites; saving money and increasing study monitoring effectiveness.
When will you start using cloud-based data collection and cloud-based monitoring as a service?
As with any new technology, there are challenges and benefits to implementing cloud technologies for your next and future clinical trials, but the benefits far outweigh the challenges of changing your modus operandi. For example, if you have ongoing clinical research, the time and cost benefits are remarkable, as you can use the same templates you originally designed and after you have amassed a collection of stored templates, and easily use pertinent data collection templates in your future studies.
The amount of flexibility and cost savings from using cloud technologies in clinical trials are vast, when compared to the clunky, standard paper-based system of clinical data management.
But flexibility and cost savings are small change.
Because Time is what counts
When data is captured in real-time, when monitoring is performed on-demand, when the information flow is online, you can reduce the time to response to deviations from weeks to hours – keeping your patients and sites and your study on track and on time.
See a large CRO perspective on how time is money