Even if you are new in pharmaceutical or medical device clinical trial industry, it is more probable than not that you recognise the value of accurate and secure data capture. After all, whether Phase I or Phase IV, the essential purpose of conducting clinical studies is to collect and manage quality data at the behest of the trial sponsor.
Product design and revisions, approval, and bringing product to market are in the hands of the sponsor company and regulatory agencies – clinicians and monitors in trials have a rather simple task regarding data, but it is of paramount significance during the testing and development of a drug or device.
As simple as it sounds for the CRO team, there are indeed challenges to maintaining data security and ensuring accuracy during the lifecycle of a clinical trial. Using cloud EDC is much easier than paper-based data capture for collecting and monitoring quality data during a clinical trial, but it is only as good as the clinicians, subjects, and managers using it – simply switching to cloud EDC will not guarantee a flawless trial.
Today we are going to discuss and detail three ways to ensure that data captured using EDC will be accurate and, just as importantly, secure when conducting your next clinical trial.
1. Addressing and ensuring study participant honesty
Many clinicians, data monitors, etc. that conduct clinical trials overlook and do not consider this fact – not every trial subject is going to be honest with the CRO. We would like to think that the members of the public willing to take part in a clinical trial are doing so for the good of science, and helping with developing effective treatments for the ill. Most of them are, but sadly, not 100% of the trial applicants are honest, and sometimes withhold information that will compromise the study’s data accuracy. For example, during a drug trial, if a patient is recreationally using cocaine throughout the study, the clinicians may notice a false positive that the drug cause high blood pressure as a side effect.
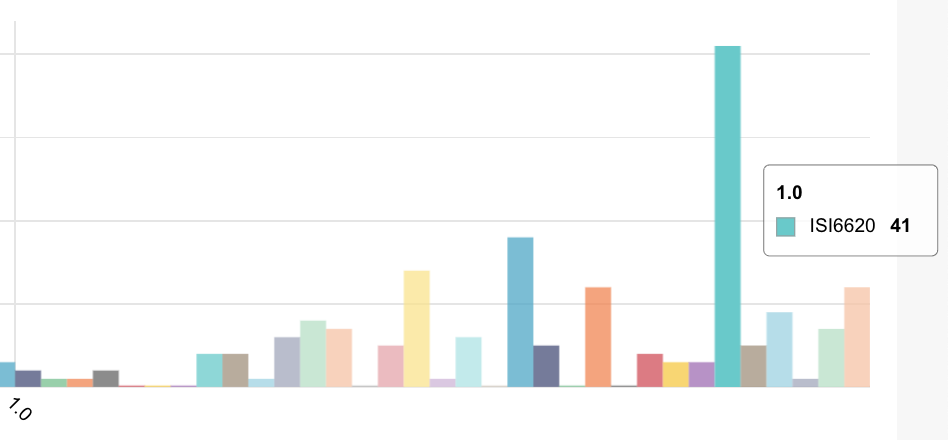
Let’s be honest ourselves for a moment – some study applicants only want to participate because of the compensation. In an NIH survey, the following numbers were discovered concerning subject subversion:
32% conceal preexisting health problems
28% conceal prescription drug use
20% conceal recreational drug use
25% exaggerate symptoms to qualify
14% falsely claim health issues to qualify
People lie – it’s a fact. Money is terrific motivator for deception, but there are ways to enhance subject screening to determine whether the applicant is the real deal, or just needs the cash from participating in the study. Keep in mind, that besides contributing to data inaccuracies, subversive and deceptive study subjects are also putting themselves at risk, so dishonest study participation goes beyond inaccurate data collection as a serious study concern.
So we do not take up too much of your time reading this post, just know that there are dozens upon dozens of ways to incentivize patient honesty, and screen whether or not a study applicant is likely to be taken at their word. Here is one quick example – during screening, mention to applicants that your external monitoring is intensive, and may require a physical monitoring device to ensure patients are following the habits and behavior standards required for the study. Patients that inform screeners that they have no issue with such are more likely to be honest during their application and following study participation.
That was just one example for screening patient honesty or subversion, but look into what would be the best methods for your own studies.
2. Do not rush EDC system design
In many cases – and one of the profound virtues of EDC – once the software is designed for an approaching clinical trial by the vendor alongside the CRO, it is a “set it and leave it” situation. What we mean is, that once the eCRFs (electronic case report forms), risk-based monitoring logic and 21 CFR Part 11 compliance validation is agreed upon to be in line with study SOPs, the EDC can be re-implemented for future studies of a similar nature with minor adjustments.
That being said, the second most crucial element (behind only FDA regulatory compliance) during software design is data quality assurance and edit checks in the eCRFs.
One of the primary reasons why paper-based systems are being replaced by EDC is that entry errors, incomplete forms, and/or illegible data submissions are circumvented by the checks. However, if software design is rushed, CROs can end up with a flawed system or one that does not have format checks in place for every data field. When this is the case, a study will go on with faulty data. Once the errors are observed, the time spent going back, editing the data, and redesigning the software negates the time-saving value of using EDC in the first place.
So, make sure that time is allocated and budgeted for pre-trial EDC design, and have your team in tandem with the vendor double check every facet of the eCRFs, and other software components. Spend a couple extra weeks during design, to save you months (or years) in the future.
3. Diligently monitor personnel changes & EDC access
Many studies, especially Phase III & IV, can carry on for years, even decades. Study staff will come and go over the course of a trial. Clinicians, monitors, and managers will all have unique levels of access to your EDC, and some will have access to editing data or changing access permissions.
To ensure data security on-premise or remotely, have a person assigned to monitoring additions and removal of study personnel, and appropriately add or delete accounts as follows. More often than not, if an employee leaves the CRO it will be on amicable terms. However, even so, mobile devices (which are commonly used for data capture/management with EDC) can be lost or stolen.
Make sure that staff are made aware to report a lost or stolen device to the CRO and to change the password as soon as notified, so that no unauthorized eyes have access to patient or trial information. Further, make certain that as soon as personnel depart from working on studies, they are swiftly removed from EDC access.
EDC trials are what you make of them
Keep in mind, it is called “electronic data capture” for a reason – data is the lifeblood of clinical trials. When there are even doubts concerning data accuracy or security, the entire clinical trial lifecycle becomes an arduous journey to undertake.
EDC offers myriad benefits for clinical studies, but the software will not conduct a flawless trial on its lonesome. Use these tips to take advantage of all that EDC has to offer, and keep your data safe, secure, and reliable.
Posted by: David Tashjian